In a world where many of us are increasingly afflicted with chronic, acute, and inflammation-related pain, it is easy to find our entire lifestyle and even our relationships badly affected by symptoms of pain, and all types of pain. However, many studies have been conducted which indicate CBD for pain and inflammation may show some clinical promise. While most experiments and research has been conducted on rodents, others have involved humans, and have led to the encouraging conclusion that CBD may have the potential to affect pain and sleep quality. While further research is needed, it is important to examine the possible impact of CBD for inflammation and other types of pain.

We might describe pain broadly as an unpleasant experience of hurt or discomfort. The sources of pain are many and varied, from emotional suffering to mental distress, from acute physical damage to chronic medical conditions. Pain stabs, throbs, aches, and pinches are all common pains we may feel at any given point in life. It sometimes correlates with a host of other undesirable sensations, such as nausea, dizziness, and fatigue. Persistent pain can affect a person’s entire lifestyle and relationships–and that is rarely, if ever, for the better.
But there are some questions we have about pain: what is it, how does it occur, and perhaps most importantly, how can we prevent it? We have all heard the expression ‘no pain, no gain,’ but we would hardly consider all types of pain as equally necessary. Not all painkillers are alike, either. In this article, we are going to focus on a product that has been gaining increasing attention as an effective, safer alternative to opioid painkillers: CBD, or Cannabidiol. First, however, a little detour into the science of pain is in order.
Pain: Some Key Definitions
As it turns out, trying to understand pain is one of medicine’s oldest challenges, and research in this field still confronts many unanswered questions. For a very long time, Western medicine has tended to regard pain mostly as a symptom of some underlying health condition. Sure enough, pain’s signalling role serves an all-important function, telling us something is wrong, and that, yes, we should be getting that check. Since the mid-twentieth century, however, scientists began considering pain as a condition in its own right, with its own definitions and taxonomies.
The most well-known among these are acute and chronic pain. The expression ‘acute pain’ usually refers to the previously mentioned signal for an injury or disease. Inflammation, burns, and trauma are all examples of pathologic processes that can result in acute pain, which may be particularly relevant here for its rather obvious causes, short-term duration, and generally severe and intense manifestations.
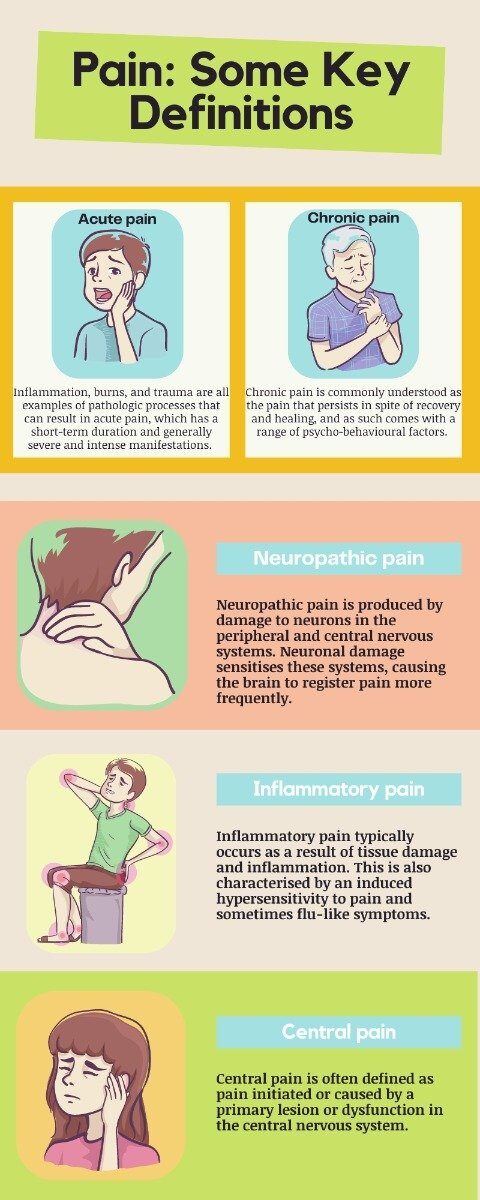
Chronic pain, on the other hand, is commonly understood as the pain that persists in spite of recovery and healing, and as such comes with a range of psycho-behavioural factors. Chronic pain is becoming increasingly accepted as an autonomous pathology to be understood in its own right–rather than simply in opposition to acute pain.
Other key categories include:
- Neuropathic pain, which is produced by damage to neurons in the peripheral and central nervous systems. Neuronal damage sensitises these systems, causing the brain to register pain more frequently. Neuropathic pain is often described in terms of burning sensations, as well as excruciating pins and needles. Examples of neuropathic pain include post-herpetic (post-shingles) neuralgia and components of cancer pain.
- Inflammatory pain, which typically occurs as a result of tissue damage and inflammation. This is also characterised by an induced hypersensitivity to pain and sometimes flu-like symptoms. Examples of inflammatory pain include those associated with arthritis and postoperative pain.
- Central pain, which is often defined as pain initiated or caused by a primary lesion or dysfunction in the central nervous system (such as may happen with tumours, or multiple sclerosis). Central pain may be considered a subtype of neuropathic pain, though research suggests that there are many types of ‘central pain syndromes’ (CPS) with distinct features.
It is important to bear in mind that these categories are not mutually exclusive. For example, chronic pain can involve a mix of inflammatory and neuropathic components. Things get even more complicated when you consider that chronic pain has social and demographic factors on top of biological and psychological ones- but those are tales for another time.
Why do we feel pain?
When it comes to pinning pain down to its core components, we must let go of the simplistic idea that all pain results from identifiable causes working through universal pathways. Pain is a complex phenomenon, and perceived pain cannot always be explained on the basis of neurological or somatic processes. As the neurologist V S Ramachandran put in an insightful article on the lingering mysteries of pain: “There is no direct hotline from pain receptors to ‘pain centres’ in the brain. Even the mere visual appearance of an opening fist can actually feed all the way into the patient’s motor and touch pathways.” That’s right: we can feel pain that is ‘not there,’ just as research has shown the same injury can feel less painful depending on whether we are in a safe and protected environment, or in a state of ongoing anxiety and distress.
Of course, some of the stuff about how pain works we do understand, or at least we think we do. Touch a hot surface, and skin receptors will quickly send electrical nerve impulses to the spinal cord (i.e., the central nervous system) via sensory neurons, where the impulses are processed and registered as pain. Right? In fact, the processing of information by the brain can take a little too long (we are talking 130-160 milliseconds), which can be enough to burn you badly on the stove. With such extreme stimuli as heat, then, sensory nerves are usually short-circuited, allowing you to more quickly pull your hand to safety.
With most kinds of pain, however, such bypassing of the brain is unlikely to occur. The whole process becomes then far more interpretive, with nerve messages signalling dangers–rather than ‘pain’ as such–and reactions that depend on a number of contextual and subjective factors.

This ‘subjective’ component does not mean that we can simply ‘think ourselves out of pain’. We might think of pain rather like blushing: we can never totally control it. Chronic pain offers a case on point: the injury is healed, but the pain persists. You can be as calm and optimistic an individual as any, and even meditate twice a day, but if you suffer from chronic pain, chances are that painkillers will be one of your only options.
Fortunately, relieving and killing pain does not require that we fully grasp the intricacies of pain perception. What we must remember though, is that not all ways of getting rid of pain are equally advisable, or safe. In this article, we are going to focus on the most notorious class of painkillers – opioids – and consider the pros and cons of using cannabinoids and CBD products as an alternative supplement.

Bad Opioids vs. Good Cannabinoids: Is It Really That Simple?
Back in the 1990s, general medical opinion had it that opioids could treat any kind of pain– provided that the dose was high enough. Opioids became the most prescribed class of medications in the US, with some devastating effects on public health. You may be familiar with the ‘opioid addiction crisis’ in the US, which has seen thousands of lawsuits filed that allege pharmaceutical companies fueled a healthcare disaster responsible for hundreds of thousands of uprooted lives from 1999 to 2017. In brief, more and more people came to rely on opioids for treating all sorts of pains, often ignoring their multifaceted nature, or the fact that effective solutions may lay in lifestyle changes. Addiction to opioids grew dramatically, as did opioid-related deaths.
Though it pays to probe beneath the bad reputation of opioids and understand how they work on the body, it has become clear that their strong analgesic effects involve too high a cost in the long run. CBD, on the other hand, can have analgesic effects without any of the toxic, addictive, and potentially deadly complications of opioids– hence one of the reasons why CBD and cannabinoid products have been on the rise. When it comes to relieving pain, it would then seem that cannabinoids are the future, and opioids the past. But what evidence is there to support these claims so often boasted by CBD wellness companies? Are opioids and cannabinoids really all that different, with one toxic and bad, the other natural and healthy?
Interestingly, the discovery and use of both opioids (like morphine and codeine) and cannabinoids (like THC and CBD) have deep roots in human history. The first class of substances derive their active ingredients from opium, which is itself extracted from poppy seeds (Papaverum somniferum), with morphine being the most active ingredient. Cannabinoids are instead found in the cannabis plant (Cannabis sativa), with THC being the most prevalent compound, followed by CBD. Those cannabinoids found naturally in cannabis are known as ‘phytocannabinoids’ (from the Greek phuton, ‘a plant’), as opposed to cannabinoids synthesised in a lab (‘synthetic cannabinoids’). A similar distinction holds between ‘opiates’ and ‘opioids,’ respectively. Morphine– which remains today the most widely-used painkiller in medical practice – is technically an opiate, or an ‘opium alkaloid,’ from which a number of semisynthetic drugs, like hydromorphone, or synthetic ones, like heroin, may be derived.
There is a third class of cannabinoids and opioids: namely, those biosynthesised naturally by our bodies. ‘Endogenous opioids,’ as they are called, play a key role in analgesia and nociception (the perception or sensation of pain), as well as in regulating numerous physiological functions, such as responses to stress, respiration, and immune functions. Endocannabinoids are also known to play a host of physiological roles, including the regulation of mood, metabolism, pain sensation, and the immune system. At a basic level, endocannabinoids are neurotransmitters that bind to receptor proteins. So are endogenous opioids. Put in this fashion, it becomes apparent that opioids and cannabinoids have more than a few things in common.
Far from meaning that cannabinoids have the same properties as opioids, what their pharmacological similarities entail is these substances’ ability to interact on a number of levels. Though research on these interactions gets predictably quite complicated, recent studies have concluded that cannabis may play a key role in alleviating opioid withdrawal symptoms and decreasing the likelihood of relapse.

Yet other studies show that patients using opioids for chronic pain decreased their use by 40-60% after being given access to cannabis. The same patients also reported fewer side-effects and displayed an interesting improvement in cognitive function. These growing bodies of research suggest that the synergy produced by cannabis and opioids could help achieve clinically relevant pain relief with small doses of opioids, thus helping to prevent physical dependence and dose escalation. In other words, cannabinoids are not simply the ‘good guys’ and opioids the ‘bad guys:’ they may actually work quite well together to help patients.
That being said, voices in the scientific community have pointed out that easing opioid consumption or curbing its effects with cannabis is not enough to resolve the current opioid crisis. New therapies are needed, from standard practices of acupuncture and massage, to cognitive-behavioural treatments, to other naturopathic remedies. Moreover, though key cannabinoids such as THC may work well as pain relief, we must remember that THC comes with a range of toxic side effects, especially when smoked.
This is where CBD might really make a difference. Though scientific research on the benefits of CBD, and on cannabinoids in general, is still lagging far behind opioid research, early results have been promising.

We have seen before that CBD (Cannabidiol) is one of the key phytocannabinoids. You may have heard all about this compound, or simply caught rumours about its miraculous benefits. Indeed, CBD is experiencing a surge in popularity, and wellness companies have been quick to jump on the CBD bandwagon, marketing this ingredient through everything from CBD food and chocolates to CBD bath bombs, lotions, and of course, CBD oils.
Looking at all of the different uses and effects that CBD has been attributed falls beyond the scope of this article. Something worth mentioning is that research around CBD strongly supports its use in treating some of the cruellest childhood epilepsy syndromes. CBD has been shown to potentially work where some antiseizure medications may fail, a success that was recently crowned by the release of the first-ever FDA-approved cannabis-derived medication, Epidiolex, which contains CBD.
Other notable uses for CBD include help in supplementing anxiety and sleep-related problems. A recently conducted study showed that, out of 72 adults suffering from either anxiety or poor sleep, 79.2% experienced a decrease in anxiety scores within the first month of CBD treatment, while sleep scores improved in 66.7% of patients– albeit with fluctuating results. 3 out of the 72 subjects, it should be noted, did not tolerate CBD well– which makes for a good reminder that you should consult your doctor or physician before supplementing your health with CBD!

A study from the European Journal of Pain examined the efficacy of applying CBD topically for the reduction of inflammation pain associated with arthritis in rodents. The results: after 4 consecutive days of applying CBD gels, investigators noticed a significant reduction in joint swelling, with changes in limb posture scores indicating a reduction in inflammation-related pain. Application of the gels further led to a contingent thickening of the synovial membrane (a layer of connective tissue between joints and tendon sheaths).
Yet another study has reported that systemic administration of CBD into rodents’ spinal cords significantly suppressed chronic inflammatory and neuropathic pain. Together, these studies clearly suggest that CBD may aid in the treatment of chronic pain. We should note that these experiments were all conducted on rats, which always makes a straightforward extrapolation to human subjects rather tricky.
The one placebo-controlled, parallel-group study conducted so far to test the effectiveness of CBD for neuropathic pain relief makes use of a nasal spray with equal amounts of CBD and THC. The findings from this study, however, demonstrated clinically important improvements in pain and sleep quality. In the end, we can only conclude with one of the maxims of all scientific inquiries: ‘more research on this subject is needed.’
The little available evidence we have holds great promises. But as with all promising talents, CBD’s must be nurtured with care. The sad truth is, that the boom of CBD wellness products has yet to be followed by a parallel concern with regulation and quality control. We thus recommend that you only go for CBD products that have been tested by third-parties, and more: that you make sure to double-check products’ certificates of analysis (COA) for anything suspicious.
The day when scientists will have uncovered all of the beneficial effects of CBD is still somewhere in the future. Waiting can be a pain, but if we manage to ensure quality research and production, it is only a matter of time before CBD becomes widely accepted as a pain remedy. In the meantime, make sure to keep yourself informed. This article has barely scratched the surface of the complex world of CBD and cannabinoids–if you crave more, read on and dig deeper into our Alphagreen Academy features.

Anastasiia Myronenko
Anastasiia Myronenko is a Medical Physicist actively practicing in one of the leading cancer centers in Kyiv, Ukraine. She received her master’s degree in Medical Physics at Karazin Kharkiv National University and completed Biological Physics internship at GSI Helmholtz Centre for Heavy Ion Research, Germany. Anastasiia Myronenko specializes in radiation therapy and is a fellow of Ukrainian Association of Medical Physicists.